

Health in all policies approaches, for example-where health impacts are considered in policy processes across government-have been developed by governments in Europe, Canada, and elsewhere. Cross-sector partnerships have been proposed as a way to coordinate these activities to improve people’s health.Ĭollaboration between sectors to improve health is nothing new. These factors, in turn, are influenced by the activities of multiple organizations and groups, such as national and local governments, social services agencies, schools, and employers. While access to health care is an important part of this picture, wider non-medical factors, such as education and income, play a major role in shaping health and its distribution. Population health is influenced by a broad range of factors-including structural social and economic conditions, public policies on education, social security, health care, and other areas, living and working environments, and more.
The reasons for this are not hard to find. Ultimately, local collaborations should be understood within their macro-level political and economic context, and as one component within a wider system of factors and interventions interacting to shape population health.Ĭollaboration between health care, social services, and other sectors is increasingly seen as a route to improving health and health equity. The benefits of collaboration may be hard to deliver, hard to measure, and overestimated by policymakers. But we know little about which kinds of collaborations work, for whom, and in what contexts. In theory, collaboration between local health care and non-health care organizations might contribute to better population health. But data linking factors in these domains to collaboration outcomes is sparse. We grouped these into five domains: motivation and purpose, relationships and cultures, resources and capabilities, governance and leadership, and external factors. Despite this, many studies report on factors associated with better or worse collaboration. And evidence of impact on resource use and spending are limited and mixed. Evidence of impact on health services is mixed. Overall, there is little convincing evidence to suggest that collaboration between local health care and non-health care organizations improves health outcomes.
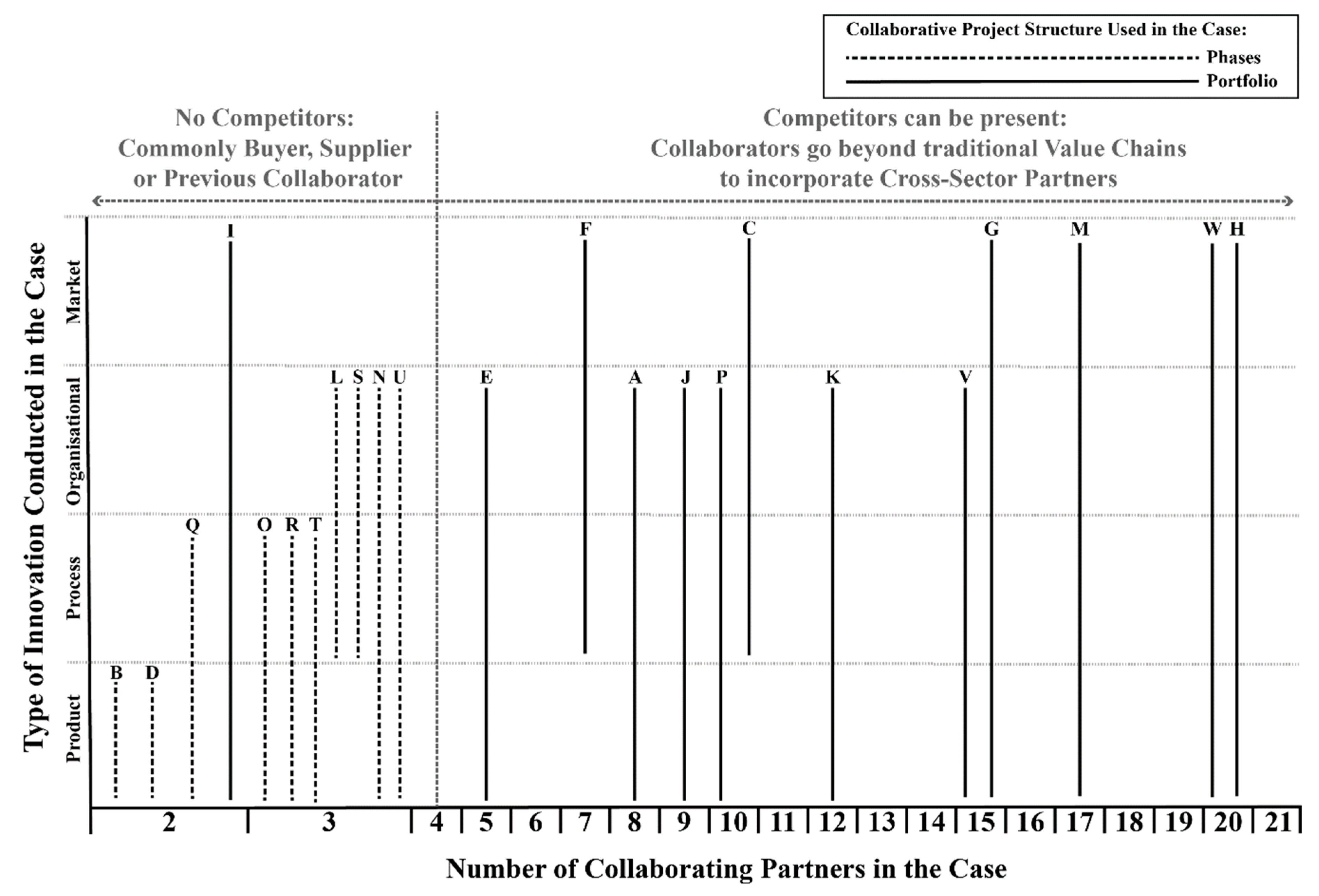
Others focused on collaborations with a narrower focus, such as better integration between health care and social services. Some studies included data on collaborations with broad population health goals, such as preventing disease and reducing health inequalities. The 36 studies we reviewed included evidence on varying forms of collaboration in diverse contexts. We used a narrative approach to synthesizing and reporting the data. We assessed risk of bias in the studies using standardized tools. We extracted data from these studies and used Nvivo 12 to help categorize the data. We searched four databases and included 36 studies (reviews) in our review. We carried out a systematic review of reviews to synthesize evidence on the health impacts of collaboration between local health care and non-health care organizations, and to understand the factors affecting how these partnerships functioned. Yet little is known about the impact of cross-sector collaboration on health and health equity. Local collaborations have been developed for decades.
#NVIVO 12 COLLABORATION DOWNLOAD#
Each download is good for one academic year and can be reactivated as needed each fall on or after August 1.Policymakers in many countries promote collaboration between health care organizations and other sectors as a route to improving population health.


 0 kommentar(er)
0 kommentar(er)
